A Virginia Commonwealth University team is developing an affordable, noninvasive treatment for respiratory distress syndrome that can be delivered without the need for complex medical equipment, supported by a $3 million grant from the Bill & Melinda Gates Foundation.
RDS occurs in newborns who lack natural surfactants - materials that reduce liquid surface tension, enabling carbon dioxide and oxygen to easily exchange as lungs expand and contract, oxygenating blood and facilitating the body’s natural functions. Though treatable through external therapy, the current procedure’s cost, complexity and invasiveness make it inaccessible to many who require it, especially infants in low- and middle-income countries.
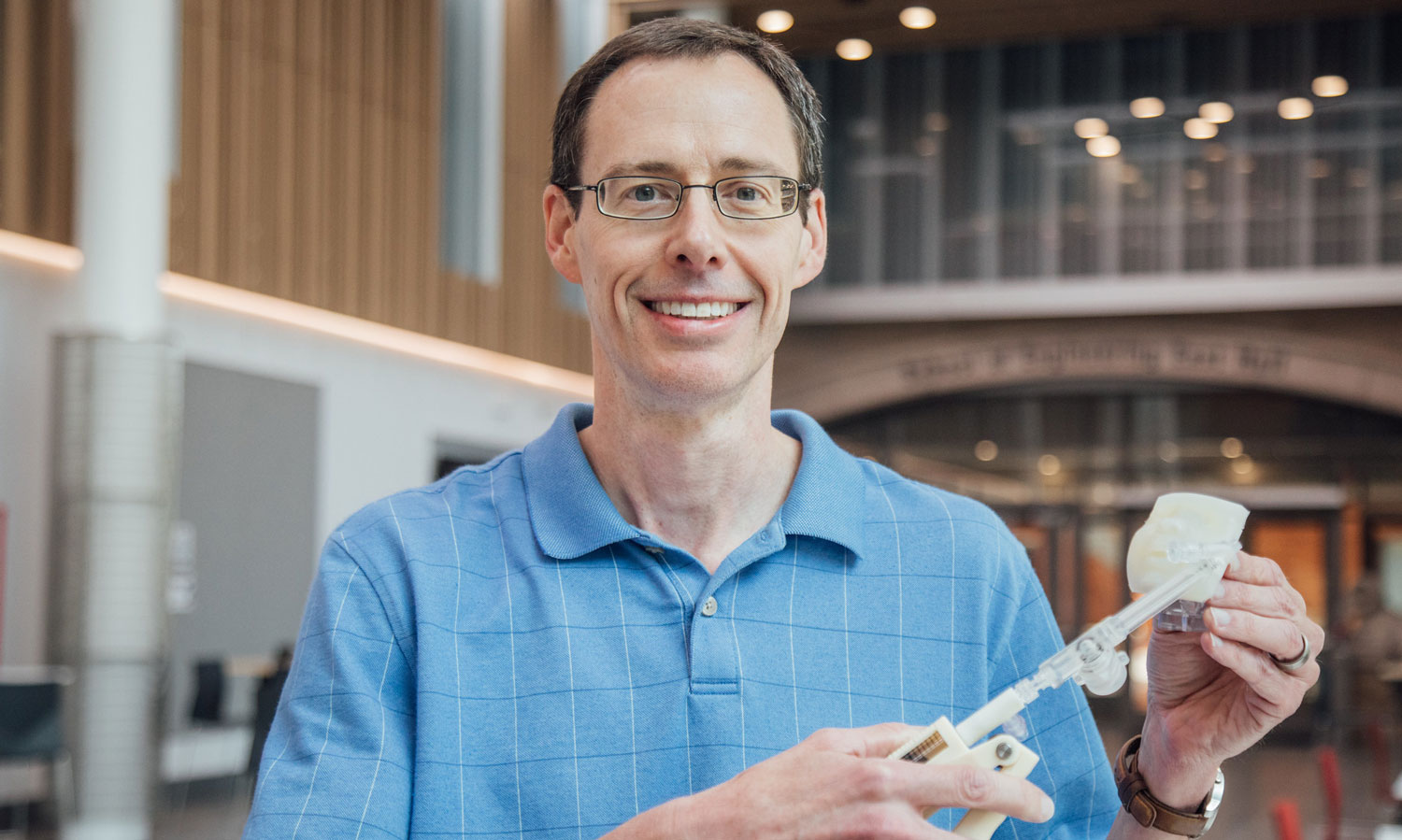
This grant is helping Worth Longest, Ph.D., the Louis S. and Ruth S. Harris Exceptional Scholar Professor in the Department of Mechanical and Nuclear Engineering in the College of Engineering, and his colleagues create a surfactant that can be aerosolized and a device to deliver it.
Current RDS treatments involve administering sedation for intubation and instillation of liquid surfactant into the lungs. In settings where surfactant administration is available, doctors must weigh these additional risk exposures prior to making the decision to give surfactant even when it is likely to be beneficial. When combined with the need for specialized equipment operating in a sterile, temperature-controlled environment, access to this life-saving treatment becomes inaccessible due to either cost, availability of proper facilities or both.
This need led Longest to partner with Michael Hindle, Ph.D., Peter R. Byron Distinguished Professor at the VCU School of Pharmacy, and Rob DiBlasi, leading clinical researcher and principal investigator at Seattle Children’s Research Institute, to seek funding from the Gates Foundation in order to develop an aerosol drug formulation and delivery mechanism for a synthetic lung surfactant capable of being delivered anywhere, with minimal equipment and at a reasonable cost.
“Some physicians regard aerosolized surfactant delivery as an obvious need in neonatal respiratory care,” Longest said. “It’s been envisioned for many years, but has not been realized due to a number of obstacles.”
Among the challenges is how to deliver an effective dosage of the aerosol formulation. Current dry powder inhalers require more air to operate effectively than can be administered to an infant based on their smaller lung capacity. These inhalers also are limited to about 1 milligram of medication, significantly less than is required for surfactant treatment.
Longest and Hindle will use their expertise in designing aerosol delivery systems to engineer an effective delivery method. Using 3D-printed upper respiratory pathway models, the team can test the effectiveness of a dispersal mechanism to ensure the dry powder formulation is being delivered deep within the lungs at the required high dosage. Formulation of the dry powder medication used by the team's delivery mechanism is led by Hindle. It involves using a sound energy bath to mix a combination of ingredients before employing a spray-drying technique to convert the liquid into a powder, which can then be aerosolized.
Inline dry powder inhalers previously developed by the Longest and Hindle labs demonstrate the capacity to achieve proper powder formulation dispersion with a low air volume. Their teams received a patent for this technology in July and are applying the same strategy to a surfactant formulation that can be aerosolized.
“Because these delivery mechanisms are strongly linked to the drug formulations they are designed to administer, it’s important to perform this kind of research simultaneously and in an iterative manner,” Longest said. “My lab collaborates with Dr. Hindle’s lab on a daily basis to solve this and other challenging problems in the field of pharmaceutical aerosols.”

Work is currently underway with refinement of the delivery mechanism, followed by validation using computational fluid dynamics and concurrent lab testing to explore different design alternatives. The goal is a high-efficiency rapid aerosol delivery product that can fully restore an infant's blood gas levels and be administered as a stand-alone therapy in less than one minute, or simultaneously during nasal continuous positive airway pressure, or CPAP, therapy.
The team will also employ unique 3D-printed airway models that replicate the anatomy of preterm infants with the goal of expanding the age range of treatment and preparation for commercial production. Concurrent with this research will be development of a larger spray-drying system for producing the dry powder surfactant formula. The proposed devices, strategy and formulation are also based on earlier and ongoing work by Longest and Hindle funded by the National Institutes of Health.
“Though we have a strong foundation for what we want to accomplish, there is much work to be done,” Longest said. “This is a multi-year project that will involve collaboration between several teams with a focus on developing treatment accessible to low-resource populations, which will be supported by grant funding from the Gates Foundation.”
Among the researchers working with Longest are Dale Farkas and Sarah Strickler, two former VCU undergraduates who returned to VCU as part of the mechanical and nuclear engineering Ph.D. program. Working with an established group of aerosol researchers is also what brought Longest to VCU.
“As an engineer, I want to use my training to have a positive impact on people’s lives,” Longest said. “Many elements of my skill set line up well with the treatment of respiratory diseases, and I came to VCU almost 20 years ago based on the opportunity to work with the School of Pharmacy Aerosol Group, including Drs. Hindle and Peter Bryon, who is now retired, as well as the chance to be a part of a young and growing engineering program.”
Longest is now part of a strong and established collaboration between VCU’s College of Engineering and School of Pharmacy. Foundational research performed by his Aerosols in Medicine Lab enables existing treatments to be reengineered for new challenges, such as developing products for treating premature infants with RDS in low-resource populations.